By Michaela Wrong
The neurosurgeon stepped back from the control panel and, for a moment, all went still as we listened to the strange music filling the operating bloc. A river was rushing down a mountain, tumbling in a white frenzy over rocks, cascading into icy green pools. Or so it sounded. In fact we were sharing what must surely count as one of the most intimate of human experiences, more intimate than sex or childbirth: we were listening to Michael's mind, its electrical activity picked up by electrodes plunged deep into his brain.
It sounded like a force of nature: tireless, ceaseless, burbling with energy. But the impression was misleading. For at least the past 16 years, Michael Holman's brain has not functioned as those of other people. That fact explained why we were gathered in a room in Grenoble's university hospital last month, unrecognisable and anonymous in our blue gowns and white masks, listening to his cerebral concerto.
In his late 30s, Michael was diagnosed with Parkinson's disease, an illness which causes the brain to gradually stop producing dopamine, the chemical that transmits the brain's motor instructions to nerves and muscles. For years, like the 120,000 other Parkinson's sufferers in Britain, he had been allowed to lead something approaching a normal life by taking levodopa, the miracle drug discovered in the 1960s which acts as a partial substitute for dopamine.
Watching Michael take levodopa was like witnessing a Jekyll and Hyde metamorphosis. One moment he seemed 100 years old, shaking uncontrollably, shuffling as he walked, a fragile figure just asking to get mugged. Minutes later, as the drug kicked in, he straightened to become the man his friends remembered of old - dynamic, humorous, frighteningly incisive. With one bound, he was free.
Parkinson's, which affects one in 100 people over 65, doesn't kill you. It doesn't - in most cases - even affect your mental faculties. It just destroys your life. The longer you take levodopa, the less effect it has. Side-effects - a squirming known as "dyskinesia", which produces convulsive leg kicks and head movements worthy of a BSE-stricken Friesian - become more pronounced. By last year, Michael's "off" moments, when he would be stuck in a chair, trembling uncontrollably, were heavily outnumbering his "on" moments. Dr Jekyll was making his excuses, and Mr Hyde was taking over.
Early retirement from his job as Africa editor of the Financial Times loomed. Woken in the early hours by his own shuddering, Michael fantasised about a full night's sleep. I would cajole him into going out, only to regret such Panglossian optimism. It is not much fun watching your dining companion becoming rooted to their chair, incapable of lifting fork to mouth without flicking food at the wall. At the cinema, I could feel the split-second when his medication wore off: a gentle trembling would escalate to a full-throttle judder rippling down the row of seats. "One of these days," I'd think, "someone is going to accuse him of wanking and there will be a scene."
Increasingly, Michael simply avoided such awkwardness by staying at home, embarrassed by the stares of strangers who assumed he was drunk. With even holding a book requiring effort, existence was shrinking to a living room and a television screen.
Time was running out, yet none of the available alternatives seemed viable. A lot of excitement was being generated by research into foetal stem cells, injected into patients' brains in the hope that they would start producing dopamine. Earlier this month, crushing the hopes of millions of sufferers around the world, a Columbia University study showed that in 15% of those treated in this way, the outcome was worse than the disease, with the stem cells producing so much dopamine that patients went into uncontrollable, permanent spasms.
Another path was surgery. As far back as the 50s, doctors discovered that destroying part of the brain's basal ganglia, or thalamus, known as "lesioning", relieved many of the symptoms of Parkinson's. But Michael's specialist had long counselled him against this. Once destroyed, the brain cells would be gone for ever, ruling out any possibility of future revival.
Just as this unpalatable prospect was becoming to seem the only option, Michael began hearing about a groundbreaking surgical alternative. Getting details proved extremely difficult. But eventually we learned that neurosurgeon Alim Louis Benabid and neurologist Pierre Pollak, professors based in the French city of Grenoble, had perfected a technique in which two electrodes were inserted inside the subthalamic nucleus, an area deep inside the brain. A battery - installed in the chest like a pacemaker - then sent a low-voltage current into surrounding tissue. For reasons that remained tantalisingly unclear, such stimulation had a similar effect to dopamine.
Crucially, the treatment didn't involve burning away precious brain cells. It was reversible, which meant Michael could benefit if stem-cell treatment proved effective in a few years' time. This wasn't a cure for Parkinson's, we were repeatedly warned. But if it could alleviate the main symptoms, it would already have worked a miracle.
Why go to France? Neurosurgeons in Oxford, Bristol and Dundee were just beginning to carry out deep-brain stimulation. But Professor Benabid was undisputed master in his field, and British operations numbered in the dozens, while Grenoble had carried out over 150. If the waiting list loomed as a major issue - most French patients waited three years for the operation - funding did not. To our complete lack of surprise, Michael had been told by his specialist that the NHS would not pay for the operation, available for free under the French public health system. Whether carried out in Britain or France, the £20,000 procedure would have to be privately funded - in this case by generous FT management.
With Michael ensconced in a room in Grenoble's university hospital, boasting telephone, cable television and a view of the snow-topped Alps, it was swiftly clear we had fallen on our feet. There was none of the bureaucratic chaos or plain, old-fashioned filth experienced in a recent encounter with a London hospital. Wards were spotlessly clean, and staff consideration far greater than strictly necessary. When they said a procedure would be carried out on a particular day, it was - if not the day before. There was a special budget hostel for people visiting patients, a hospital hairdresser selling an impressive range of wigs for the newly operated, a hospital travel agency organising return trips; my God, even the food at the hospital cafe was decent.
"Be prepared. It's no cakewalk," warned a colleague who had watched a friend's father go through the procedure. She was right. But it was actually to prove far less gruelling than expected, an intense, uplifting experience which left me as rapturous and moved as a new father reeling punch-drunk from the delivery room.
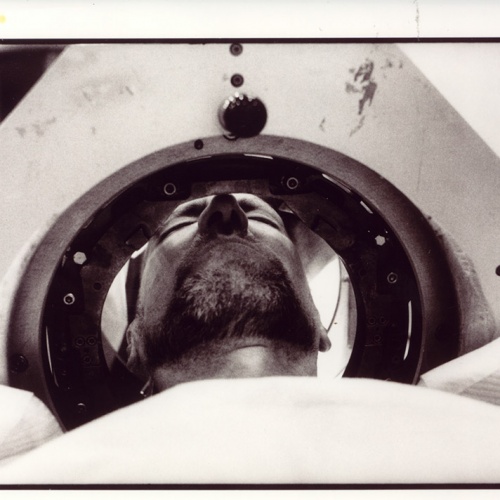
In the first of the three operations involved, Michael had his head shaved and five bolts, a little like the screws provided with Ikea shelving, drilled into his skull. The bolts meant he could be literally screwed into a rigid metal frame, ensuring his head was kept stationary during both the main operation itself and a preliminary scan to establish the exact location of Michael's brain structures.
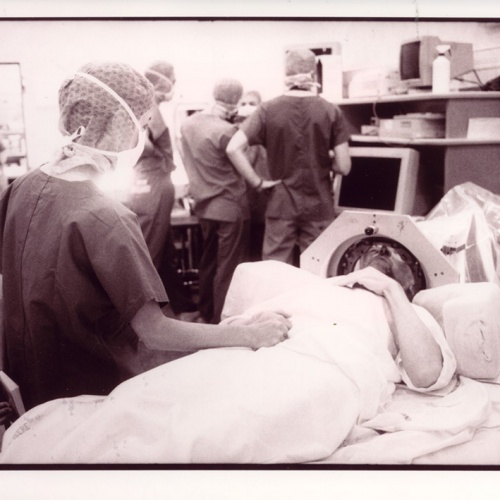
The second operation was the big one; the one teeth were gritted for and spines stiffened over. We had been warned to expect anything up to 20 hours. The previous week, a surgical team had emerged exhausted at three in the morning. Michael would have to be conscious throughout, guiding the surgeons to exactly the right spot with a running commentary on his sensations. The comforting oblivion of anaesthesia was not on offer, but Michael should not feel pain: the brain, paradoxically, does not have much sensation.
With the surgeons' blessing, we had asked if a film director friend could video the procedure and I could take notes. It was a very journalistic way of dealing with personal crisis. But there was also a practical point to the request: a video logged with the Parkinson's Society would help to ensure that others did not repeat our tedious trawl for information. In any case, I wanted to be there as possible interpreter, should Michael find himself struggling to communicate with French staff.
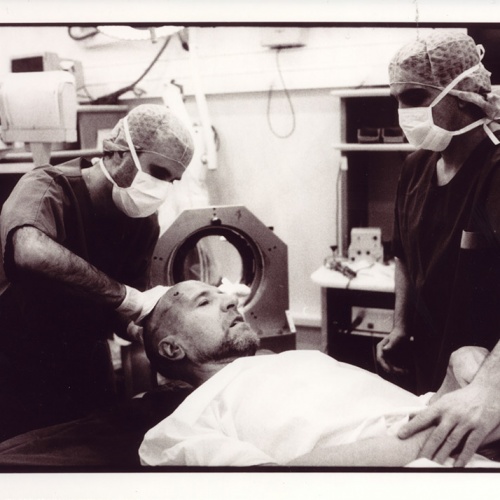
I stayed out of the operating bloc for the first few hours, warned that queasiness was most likely to strike at the start, when the surgeons used a high-pitched drill to pierce the skull. But I was called inside in time to hear the white noise of Michael's mind, picked up by five test electrodes delicately inserted through the hole in one side of his head. It is a sobering experience seeing someone you know splayed on a surgeon's table, blue-shrouded figures hovering, scalpels laid in neat rows. But there was not much blood: after all, not many tissues had been sliced into. Locked into his frame, with a physiotherapist massaging his limbs, Michael seemed cheerful and alert enough.
Over the next few hours it became clear just why the operation took so long. Using what looked like the gadget for lowering a garage door, the neurophysicians sent currents to varying depths along each electrode, painstakingly monitoring Michael's reactions and the suppleness of his joints - floppy when sensitive cells were hit, stiff when the electrode was in the wrong place. "I feel nauseous," he would say. Or: "That was like a strong electric jolt."
For minutes at a time, they would peer at his lips, watching for the slightest of tremors. The area of the brain controlling facial movement is just beyond the target area, so a trembling there was a helpful clue, indicating they had overshot. Once all electrodes had been tested, the team decided which was best positioned, then inserted a permanent one in its place. Working with the delicate precision of a sushi chef, the surgeon first patched the skull hole, then sealed it with dental cement.
If the first insertion went swimmingly, the second seemed more alarming. With one side "fixed", Michael's second side became far more sensitive. The electrical jolts sent his body flipping around on the table like a fish on a marble slab, convulsions rippling down his face. "He's not going be able to take much more of this," I thought as he wiggled and slithered. But as far as the surgeons were concerned, things were going just fine.
Indeed, we finished in just 11 hours - an ultra speedy operation. As he realised that the end was near, Michael got a second wind. Euphoric, he chattered excitedly with the surgeon stitching him about French politics, and as they finally unbolted the metal frame, he was seemingly beside himself with relief, seizing the hands of those he was convinced had released him from a 16-year hell. "The men and women who have imprisoned me have set me free," he said, and I found I had tears in my eyes. I had witnessed something very like a birth - the granting of a new life to a man who had nearly given up.
That night, leaving a hyped-up Michael to rest, I celebrated at a local brasserie with the friend who had videoed the procedure and his French soundman, who impressed us both by coolly ordering tete de veau. Deposited in front of him with a flourish, the tranche of calf's brain was an exact replica of the X-rays of Michael's brain that we had spent the day gazing at with the medical profession's finest. "Don't you think that's a bit inappropriate?" we asked him, aghast.
There was one last operation to go: the installing of a battery the size of a cigarette-lighter below Michael's collarbone, linked to the electrodes via wires snaking invisibly under his skin. Michael then spent a few weeks roaming the hospital in a wrinkled cream cap that made him look rather like an over-sized condom, as the doctors tinkered with medication and battery voltage, adjusted using a mouse held over Michael's chest.
He's not quite there yet. Boasting scars that make it look as though a shark took his head in its mouth, then thought better of it, he still has a slight tremor and does a lot of sleeping. But the dyskinesia is gone, and the interminable periods where Michael shuddered and sweated, unresponsive to drugs, are a thing of the past. He has stopped taking dopamine entirely, and dropped two of his three other key drugs: a change that in itself will save the NHS over £3,000 a year. The fact that a well-paid professional remains a taxpayer, rather than retiring early to claim disability benefit, also means the operation begins to pay its way.
Michael goes back to Grenoble in three months for fine-tuning, by which time his chicklet's fuzz will have grown into real hair. But his voice has already become more forceful: he raps out questions at machine-gun speed, as though determined to make up for years of lost time. He radiates well-being and his joie de vivre has spilled over on to those who love him. "In a way, I feel as though we've all been liberated," a Dutch friend in Kenya said over the phone the other day.
Freedom looms, and with it huge questions. Given the chance to start again, where does a 56-year-old workaholic begin? Will Michael simply put in more hours at the office? Or will he discover Buddhism, go round the world with a backpack, learn to play the piano? Anything seems possible. For the moment, he is planning to retake a long-defunct driving test and talks of a driving holiday. Where would he like to go first? Why, France, of course.